Parkinson's
EtiologyParkinson's disease (PD) is a neurodegenerative disorder that mostly presents in later life with generalized slowing of movements (bradykinesia) and at least one other symptom of resting tremor or rigidity. Other associated features are a loss of smell, sleep dysfunction, mood disorders, excess salivation, constipation, and excessive periodic limb movements in sleep (REM behavior disorder). PD is a disorder of the basal ganglia, which is composed of many other nuclei. The striatum receives excitatory and inhibitory input from several parts of the cortex. The key pathology is the loss of dopaminergic neurons that lead to the symptom. It is the seconds most common neuro-degenerative condition in the world after Alzheimer's.
The condition is caused by the slow deterioration of the nerve cells in the brain, which create dopamine. Dopamine is a natural substance found in the brain that plays a major role in our brains and bodies by messaging and therefore communicating across various systems.
The cause of PD has been linked to the
- Use of pesticides, herbicides, and proximity to industrial plants.
- After injection of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) (An accidental finding). This chemical accumulates in the mitochondria.
- Oxidation and generation of free radicals causing damage to the thalamic nuclei.
- Genes, the risk of PD in siblings is increased if one member of the family has the disorder. These cases also tend to occur much earlier in life.
- The altered function of alpha-synuclein may play a role in the etiology of PD. Current research is focussed on preventing the propagation and aggregation of alpha-synuclein
Epidemiology
- Parkinson’s most often occurs after the age of 50 and is one of the most common nervous system disorders of the aging population.
- PD affects 1 to 2 people per 1000 at any time. An estimated seven to 10 million people worldwide are living with Parkinson's.
- The prevalence increases with age to affect 1% of the population above 60 years.
- 5% to 10% of patients have a genetic predisposition.
- The incidence and prevalence of PD do increase with advancing age
- The condition is more common in men than women.
- In the UK, the prevalence of Parkinson's is 145,519 with an incidence of 18,461 in 2018.
Interprofessional Management
PD is one of the most common motor disorders worldwide. The disorder has no cure and is progressive. The condition can present with motor abnormalities and a variety of psychiatric and autonomic problems. Almost every organ is affected by this disorder, and as the disease progresses, management can be difficult. An interprofessional team approach is the best way to manage the disorder.
Some non-motor aspects (sleep problems, low mood, constipation, and loss of sense of smell) occur several years prior to observable motor symptoms develop. Physiotherapists are most often involved in the mid-stages of the condition, once balance and mobility become affected, but it can be helpful if they can assess and advise people soon after diagnosis in order to maintain activity and prevent problems.
Besides physicians, nurses, pharmacists, social workers, and physical therapists play a vital role in the daily management of these patients. Parkinson’s creates complexities for health and social staff helping individuals and those affected by it (carers, family members, friends). Managing these complex issues is a challenge due to the varied combinations of a motor (movement) and non-motor symptoms presented throughout the course of the condition.
Common Motor Symptoms that Require Management
- Tremor is a prominent and early symptom of PD (not always present and is not a necessary feature for diagnosis).
- Slowness, or bradykinesia, a core feature of PD.
- Rigidity is the third prominent feature on examination.
- A combination of bradykinesia and rigidity leads to some other characteristic features of PD, such as micrographia.
- The fourth prominent feature of PD is gait disturbance, although this is typically a late manifestation. Flexed posture, ataxia, reduced arm swing, festination, march-a-petits-pas, camptocormia, retropulsion, and turning en bloc are popular terms to describe the gait in PD. Gait disorder is not an early feature of PD but is frequently described as it is easy to recognize and cinches the diagnosis in later stages.
Complications
Depression- Dementia
- Laryngeal dysfunction
- Autonomic dysfunction
- Kyphosis leading to cardiopulmonary impairment
Prognosis
The rate of progression of the disease may be predicted based on the following:
- Males who have postural instability of difficulty with gait.
- Patients with older age at onset, dementia, and failure to respond to traditional dopaminergic medications tend to have early admission to nursing homes and diminished survival.
- Individuals with just tremors at the initial presentation tend to have a protracted benign course.
- Individuals diagnosed with the disease at older age combined with hypokinesia/rigidity tend to have a much more rapid progression of the disease.
The disorder: leads to disability of most patients within ten years; has a mortality rate three times the normal population.
Parkinson’s cannot yet be cured (treatment can improve symptoms but the quality of life is often poor). A lot of financial and other resources are being expended on research to find a cure.
Differential Diagnosis
- Essential tremor
- Huntington chorea
- Dementia with Lewy bodies
- Progressive supranuclear palsy
- Neuroacanthocytosis
- Normal pressure hydrocephalus
Aims of Physiotherapy
- Maintain and improve levels of function and independence, which will help to improve a person’s quality of life
- Use exercise and movement strategies to improve mobility
- Correct and improve abnormal movement patterns and posture, where possible
- Maximize muscle strength and joint flexibility
- Correct and improve posture and balance, and minimise risks of falls
- Maintain a good breathing pattern and effective cough
- Educate the person with Parkinson’s and their carer or family members
- Enhance the effects of drug therapy
Physiotherapy Intervention
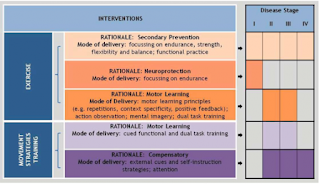
The Review version of the European Physiotherapy Guideline divides physiotherapy intervention for Parkinson’s into exercise and movement strategy training.
Exercise
Exercise has been proven to maintain health and well-being in Parkinson’s and now importantly it is shown to play a big role in addressing secondary prevention (focusing on strength, endurance, flexibility, functional practice and balance). Exercise for neuroprotection focuses on endurance and uses motor learning principles approaches, such as mental imagery and dual task training. Neuroprotection training, to be effective, should be introduced in the early stages, but helps at all stages. It involves complex, powerful and intensive exercises.
Exercise undertaken in a group setting has the added value of providing a social connection to those becoming increasingly isolated as the condition progresses, or for those who are newly diagnosed, so they can see the benefits of maintaining exercise and activity. A group environment also permits time for people to ask questions and discuss their symptoms and own management strategies with one another.
Transition Care setting improves the independence and functioning of the patients in order to delay their entry into residential aged care. provides time-limited, goal-oriented and therapy-focused packages of services to older people after a hospital stay which includes low-intensity therapy—such as physiotherapy and occupational therapy—social work and nursing support or personal care. A qualitative research study suggests better outcomes in older patients (above 80 yrs) with family participation to assist physiotherapy care in a Transition care setting.
Physical activity, in particular, aerobic exercise might slow down the motor skill degeneration and depression. Furthermore, it increases the quality of life of patients with Parkinson's. A randomized controlled trial showed favorable outcomes with exercise and horticultural intervention programs for older adults with depression and memory problems.
Randomized controlled clinical trial protocol to evaluate the effect of inspiratory muscle training on lung functions in patients with mild-to-moderate Parkinson's suggests a better outcome.
Quality of life may be increased when performing strength training against an external resistance (cycle ergometer, weight machines, therapeutic putty, elastic and, weight cuffs ...). This also improves physical parameters, such as balance, gait parameters, physical performance but the muscle strength does not improve necessarily.
Executing a dual task, e.g. talking while walking, is commonly difficult in patients with Parkinson's. Training this with Motor-Cognitive Dual-Task training, improves dual-task ability and might improve gait, balance and cognition.
A recent research study found out Progressive resistance training (PRT) to be effective in decreasing bradykinesia and improving functional performance in patients with mild-to-moderate Parkinson's Disease (PD).
Movement Strategy Training
Basal ganglia disorders cause deficits in the generation of internal (automatic) behavior. Strategies (physical or attentional cues and combined strategies) can help overcome some of the resultant problems, hence have become an increasingly utilised method of intervention for people with Parkinson’s.
Music-based movement therapy is a promising intervention that needs some further research. It is interesting since it combines cognitive movement strategies, cueing techniques, balance exercises and physical activity. The focus is on enjoying moving and not on the mobility limitation which might appeal more to the patients than standard exercises.
We can see immediately the effects of external cueing and attention on improving step length, freezing and turning during walking tasks, and in activities of daily living. A Systematic Review and Meta-Analyses suggests better outcomes with short-term physiotherapy on the symptoms of freezing of gait in Parkison's patient. However, further randomized control trial studies are still needed. Literature suggests that robot-assisted gait technology has better results in addressing the freezing of gait for Parkinson's patients. However, more research is needed in this field.
Depending on the cognitive state of the individual, they may be able to learn how to self-instruct in the use of an internal cue or strategy. If less able, the cue or strategy has to come from an external source e.g. a visual strip on the ground, the rhythmic beat of a metronome.
Depending on the stage of the condition, the rationale for intervention choices will differ:
As mentioned in the subsection on Physiotherapy for Parkinson’s: referral and assessment, during the earlier stages of diagnosis, greater emphasis is placed on education and self-management. The individual should be encouraged to continue being active and participate in physical exercise for as long as possible. Significant respiratory complications develop in many people as their Parkinson’s progresses, so attention should be paid to monitor and manage encroaching weakness of respiratory muscles and rigidity of the thoracic cage.
The European Guideline provides a section that describes the use of motor learning (pages 78 to 80), expectations if practiced and executed as a strategy to train improvements in movement. It takes the form of cued functional and dual task training, compensatory strategy training uses external cues, self-instruction and attention. Examples include:
- Visual cueing – a focus point to step over and initiate gait; strips of tape on the floor to initiate or continue walking through areas that cause slowing or freezing
- Auditory cueing – counting 1-2-3 to initiate walking; stepping to the beat of a metronome or specific music at a specified cadence to continue the rhythm of a walk
- Attention – Thinking about taking a big step; making a wider arc turn. This is applicable in case of correcting a bad habit- such as walking with stiff hip or hip hiking.
- Proprioceptive cueing – rocking from side to side ready to initiate a step; taking one step backwards as a cue ready to then walk forwards
A Systematic Review of thirty-five studies by Delgado-Alvarado M et al. emphasizes the benefit of non-pharmacological and nonsurgical treatments for freezing of gait symptoms. The study results suggest passive therapies (transcranial magnetic stimulation or transcranial direct current stimulation), active therapies (cognitive or physical training), and the transient effect therapies (using visual, auditory, or proprioceptive cues to shift the patient's habitual movements to a goal-directed one) help to overcome the freezing of gait episode.
Most people who are diagnosed with Parkinson’s are aged 50 or over, but 1 in 20 of those diagnosed are younger than this. Those with young onset of Parkinson’s are more likely to exhibit early dystonia and motor fluctuations and dyskinesias, caused by prolonged use of dopaminergic treatment.
These non-pharmalogical interventions are effective in increasing the Health-Related quality of life (HRQOL) according to Lee's meta-analysis. But since there is a big heterogenity between the interventions, more research is needed to take firm conclusions.
To deliver a patient-centered treatment, it's important to provide your patients with information and education and allow time for patients to discuss their options and ask questions. Limited clinical time may be a challenge, however, good communication and sharing information are as important as delivering an intervention.
THOSE ABOVE ALL COLLECTED FROM SOME WEBSITES
THANK YOU,
SRIKUMARAN PHYSIOTHERAPY CLINIC & FITNESS CENTER



Comments