INTRODUCTION:
Nerve injury is injury to nervous tissue. There is no single classification system that can describe all the many variations of nerve injury. In 1941, Seddon introduced a classification of nerve injuries based on three main types of nerve fiber injury and whether there is continuity of the nerve. Usually, however, (peripheral) nerve injury is classified in five stages, based on the extent of damage to both the nerve and the surrounding connective tissue, since supporting glial cells may be involved. Unlike in the central nervous system, neuroregeneration in the peripheral nervous system is possible. The processes that occur in peripheral regeneration can be divided into the following major events: Wallerian degeneration, axon regeneration/growth, and nerve reinnervation. The events that occur in peripheral regeneration occur with respect to the axis of the nerve injury. The proximal stump refers to the end of the injured neuron that is still attached to the neuron cell body; it is the part that regenerates. The distal stump refers to the end of the injured neuron that is still attached to the end of the axon; it is the part of the neuron that will degenerate but that remains in the area toward which the regenerating axon grows.
NERVE STRUCTURE:
There are two commonly used classification for PNI- the Seddon classification and the Sunderland classification.
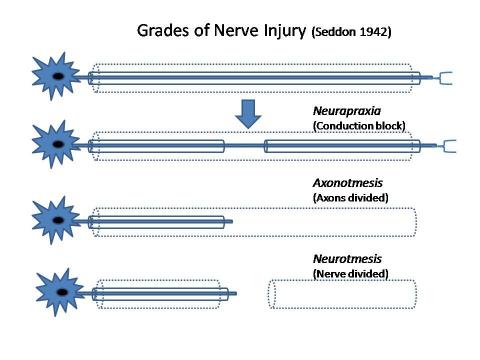
SEDDON CLASSIFICATION:
It has consists five major types of peripheral nerve injury as described in the table below:
| Seddon | Process | Sunderland |
| Neurapraxia | Local myelin damage usually secondary to compression | First degree |
| Axonotmesis | Axon severed but endoneurium intact (optimal circumstances for regeneration) | Second degree |
| Axonotmesis | Axon discontinuity, endoneurial tube discontinuity, perineurium and fascicular arrangement preserved | Third degree |
| Axonotmesis | Loss of continuity of axons, endoneurial tubes, perineurium and fasciculi; epineurium intact | Fourth degree |
| Neurotmesis | Complete physiologic disruption of entire nerve trunk | Fifth degree |
SUDERLAND'S CLASSIFICATION:
There are three basic types of peripheral nerve injuries (PNI) commonly seen in the clinic.
- Neuropraxia(Stretch related)- the peripheral nerves are elastic, but when a traction force is too strong injury occurs. If the Traction force is strong enough, a complete tear may occur, but most commonly the continuity is retained, resulting in injuries such as Erb's Palsy.
- Axonotmesis(Lacerations)-Another common type of PNI are lacerations created by blades. those types of injuries might be complete transections- but most commonly some continuity remains.
- Neurotmesis(Compressions)-The third type of PNI are compression These injuries include the Saturday Night palsy due to radial nerve compression as well as entrapment neuropathies and do not involve tearing of the neural elements.
The most common of the three is stretch-related, followed by lacerations and compression.
CAUSES:
- Peripheral nerve injuries have numerous causes including
- traumatic injuries
- infections
- metabolic problems ( one of the most common causes is diabetes mellitus); inherited causes
- exposure to toxins
- tumours
- iatrogenic causes.
Clinical presentation varies according to the nerve affected i.e sensory, motor, or combined.
Signs and symptoms may include
- Gradual onset of numbness, prickling, or tingling in your feet or hands, which can spread upward into your legs and arms
- Sharp, jabbing, throbbing, freezing, or burning pain
- Extreme sensitivity to touch
- Lack of coordination and falling
- Muscle weakness or paralysis if motor nerves are affected
- causalgia pain.
Diagnosis started from the medical history, ask about any accidents or previous surgeries, and presenting symptoms. then to do conduct a physical and neurological examination.
- Electromyography (EMG). In an EMG, a thin-needle electrode used the muscle records muscle's electrical activity at rest and in motion. Reduced muscle activity can indicate nerve injury.
- Nerve conduction study. Electrodes placed at two different points in the nerve course, measure how well electrical signals pass through the nerves.
- Magnetic resonance imaging (MRI). MRI uses a magnetic field and radio waves to produce detailed images of the area affected by nerve damage.
After a diagnosis of a peripheral nerve injury, a full subjective and objective examination is required to get a clear picture of the way the lesion is affecting the client. The examination should focus on
- Pain assessment
- Sensation deficit and skin condition
- Muscle strength/loss
- Functional deficits
- Balance deficits
- Joint stiffness
- Emotional stress
PHYSIOTHERAPY MANAGEMENT:
PAIN MANAGEMENT:
Neuropathic pain affects the quality of life and is a common consequence of nerve damage. Pain control is of paramount importance. Complete relief is rarely obtained and 40-60 % find means to obtain partial relief. A multidisiplinary approach is taken, with most input from the pharmacologist(s). Anticonvulsants and tricyclic anti-depressants are the most used drugs for neuropathic pain. A Physiotherapist can employ other modalities that show in various studies to be of benefit as complementary medicine for pain relief. These include
- massage eg aromatherapy massage, in studies, has shown to help manage neuropathic pain and increase QOL. Many differing massage techniques have been employed showing benefits for pain management and QOL.
- TENS. Application of TENS has been found to be of benefit in pain reduction in neuropathic pain. It was found to be of benefit if used at 100hz in constant mode.
- Low Level Laser Therapy (LLLT). Studies have found this to be of benefit in pain relief and acceleration of healing in treatment of neuropathic pain and neurological deficits as adjuvant therapy.
- Relaxation techniques
A consequence of denervation is muscle atrophy and functional deficits. The healthy neuromuscular junction (NMJ) is critical for nervous control of muscles. TENS has been seen in numerous studies to have a positive effect on maintaining NMJ health and in prevention of muscle atrophy. A 2018 study found the use of TENS was most beneficial if delayed to one-week post-trauma, the use of 100Hz being most beneficial.
Muscle care is of utmost importance to prevent damage to muscle units, in particular prevent:
heat or cold trauma; over stretching by gravity or incorrect lifting/transfer techniques; contractures of muscles. The below video clips give a good guide to proper handling techniques involved in passive ROM.
Techniques employed by physiotherapist to achieve the above goals are massage, US, hydrotherapy, splints, passive ROM stretches and correct transfer skill education.
When muscle strengthening exercises can commence it is important not to damage the healing nervous tissue, if pins and needles, numbness or increased pain occurs the exercise is too hard and can have a negative effect on healing.
Muscle strengthening exercises are employed as appropriate e.g isometric, graded weight progression, open-close chain. Proper splinting techniques, from the postoperative splint and cast to splints that prevent deformities,to overcome established contractures and improve function, aids in the patient's recovery. Use of support slings may be employed to assist the movement and take the weight of the limb. As may static and dynamic splints- helping to rest paralyses muscles in optimum positioning to avoid overstretching and or contractures. They also assist in allowing unaffected muscles to operate from correct positions.
A recent study found that exercise can enhance axonal growth via a neurotrophin-dependent mechanism affecting adult dorsal root ganglion neurons. Aerobic activity should also be encouraged ( aiming for 30 minutes 4 times a week) for its’ known health benefits.
FUNCTIONAL PROBLEMS:
In the relearning of functional tasks, the brain is utilized to regain visuo-tactile and audio-tactile interaction. In the upper limb, the focus is on fine motor skill learning. In the lower limb balance and coordination are areas of focus.
Sensory reeducation aids in the recovery of sensibility. In sensory stimulation pinching and tapping, brushing and icing are regularly used.
Proprioception deficits can be improved using exercise balls, balance pads for WB activities, juggling balls for upper limbs, yoga, Tai-chi.
JOINT STIFFNESS:
The soft tissues of the region and adjacent regions supplied by the damaged nerve are at risk of contractures if left in shortened positions. Regular daily massage, PROM exercises are needed on a daily basis. Protective removable static splints are also useful in contracture prevention. For joints that have become stiff ultrasound and laser are of useful therapies.
STRESS RELATED PROBLEMS:
Chronic neuropathic pain has a life-debilitating effect causing emotional stress and reduced QOL. To properly treat a client with neuropathic pain this must be respected. The ultimate goal is not simply to reduce pain but to achieve better QOL. This can only be achieved if the depression, anxiety, and sleep disorders are also addressed.
THOSE ABOVE ARE COLLECTED FROM SOME BOOKS AND
WEBSITES..
THANK YOU,
SRIKUMARAN PHYSIOTHERAPY CLINIC & FITNESS CENTER

Comments