Introduction:
This is a common cause of generalised regional pain and
disability, and is frequently associated with medically unexplained symptoms in
other systems. The prevalence in the UK is ~2–3%. It increases in prevalence
with age, to reach a peak of 7% in women aged over 70.
There is a female predominance of ~10 : 1. Risk factors include stressful
life events, such as marital disharmony, alcoholism in the family, injury or
assault, low income and self-reported childhood abuse. No structural,
inflammatory or metabolic abnormality has been identified, although
abnormalities of non-rapid eye movement (REM) sleep and of central pain
processing have been postulated as potential aetiological factors.
Clinical features
and investigations
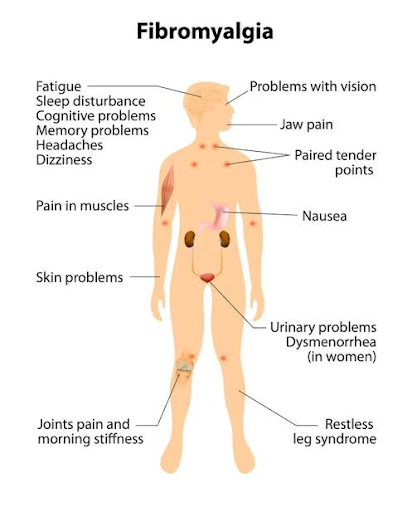
The main presenting feature is multiple regional pain, affecting the neck, back, both arms and both legs; it is unresponsive to analgesics and NSAIDs.
Patients commonly report fatigability, particularly in the morning, and reported disability is often marked. Although people can usually dress and groom themselves, they may struggle with daily tasks such as shopping and housework, and may have given up work because of pain and fatigue.
Non-locomotor features include tension headache, irritable bowel syndrome and irritable bladder.
Examination usually reveals hyperalgesia at multiple specific tender
sites. Moderate pressure at each site may be uncomfortable in a normal subject
but in fibromyalgia it produces a wince/withdrawal response. Although there are
no abnormal investigations associated with fibromyalgia, it is important to
screen for alternative musculoskeletal conditions.
Management
The patient should be reassured that the widespread pain does not reflect
inflammation, tissue damage or disease. Low-dose amitriptyline with or without
fluoxetine may be useful. Graded exercise may improve well-being. Relaxation
techniques and coping strategies employing a cognitive behavioural approach
should be encouraged. Patient organisations can provide valuable support.


Comments