Introduction:
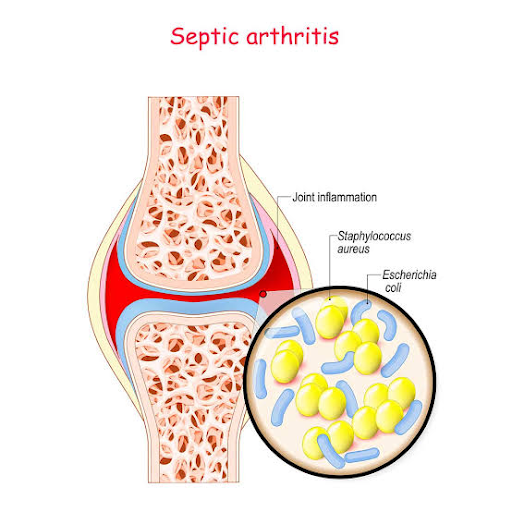
Septic arthritis is a medical emergency. It usually arises from
haematogenous spread of bacterial infection from another site, commonly the
skin or upper respiratory tract. Infection from direct puncture wounds or that
secondary to joint aspiration is uncommon. Risk factors for septic arthritis
include increasing age, pre-existing joint disease (especially RA), diabetes
mellitus, immunosuppression and IV drug misuse.
Clinical features
The usual presentation is with acute or subacute monoarthritis. The
joint is usually swollen, hot and red, with pain at rest and on movement. The
knee and hip are the most common sites. The usual culprit organism is Staphylococcus aureus. Disseminated gonococcal infection is another cause
in young, sexually active adults. This presents with migratory arthralgia and
low-grade fever, followed by the development of oligo- or monoarthritis.
Painful pustular skin lesions may also be present. Lyme disease and brucellosis
are less common causes of septic arthritis.
Investigations
Joint fluid aspiration for Gram stain and culture is essential,
under image guidance if deep. Aspirated fluid often looks turbid or
bloodstained.
Blood cultures may be positive due to bacteraemia. Blood tests may
reveal leucocytosis with raised ESR and CRP, although these may be absent in
elderly or immunocompromised patients.
Concurrent cultures from the genital tract are indicated if
gonococcal infection is likely.
Management
●
Pain relief.
●
IV antibiotics: IV flucloxacillin
2 g three times daily is first choice until identification of the organism and
its sensitivities is possible. IV treatment is usually continued for 2 wks,
followed by oral treatment for a further 4 wks.
● Daily joint aspiration in the initial
stages to minimise the effusion. If this is unsuccessful, surgical drainage may
be required.
●
Early mobilisation.


Comments