INTRODUCTION
De Quervain's Tenosynovitis is a painful, inflammatory condition caused by tendons on the side of the wrist at the base of the thumb. Pain, which is the main complaint, gets worse with abduction of the thumb, a grasping action of the hand, and an ulnar deviation of the wrist. Thickening and swelling can also be present.
Causes:
- The most common cause is chronic overuse.
- Activities such as golfing, playing the piano, fly fishing, carpentry, or activities by office workers and musicians can lead to chronic overuse injuries.
- The classic patient population is mothers of newborns who are repeatedly lifting their baby with their thumbs radially abducted and wrists going from ulnar to radial deviation.
- Repetitive gripping, grasping or wringing of objects can cause inflammation of the tendons and tendon sheaths which narrows the first dorsal compartment limiting motion of the tendons. If left untreated, the inflammation and progressive narrowing (stenosis) can lead to scarring that further limits thumb motion.
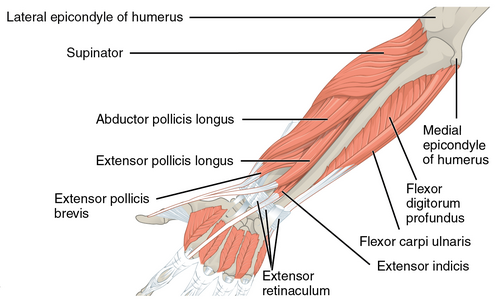
- De Quervain's has been "attributed to myxoid degeneration (the process in which the connective tissues are replaced by a gelatinous substance) with fibrous tissue deposits and increased vascularity rather than acute inflammation of the synovial lining. It is for this reason that is thought to be a tendinosis rather than a tendonitis. This deposition of the fibrous tissues causes thickening of the tendon sheath, and this can entrap the abductor pollicis longus and extensor pollicis brevis tendons and cause pain.
De Quervain's syndrome affects the extensor pollicis brevis (EPB) tendon and the abductor pollicis longus (APL) tendon. These muscles are located on the dorsal side of the forearm and go to the lateral side of the thumb through a fibrous-osseous tunnel made of the processus styloideus radii and the extensor retinaculum. The tendon sheaths around the abductor pollicis longus and extensor pollicis brevis pass through the fibro-osseous tunnel located along the radial styloid at the distal wrist.
- Extensor pollicis brevis (EPB)
- Origin: ½ dorsal side of the radius, the membrana interossea
- Insertion: base of the proximal phalanx of the thumb
- Function:
- Wrist joint: radial abduction
- Thumb: extension
- Innervations: posterior interosseus branch of N. radialis
- Artery: A. interossea posterior
- Abductor pollicis longus (APL)
- Origin: dorsal side of the radius and the ulna, the membrana interossea
- Insertion: base of ossis metacarpi
- Function:
- Wrist joint: radial abduction
- Thumb: abduction
- Innervations: posterior interosseus branch of N. radialis
- Artery: A. interossea posterior
- Overuse injury vs acute trauma
- Prior history of symptoms
- Repetitive movements of the upper extremity with work or activities of daily living (ADL)
- Hand dominance
- Pregnant or currently in the post-partum stage
- Pain:
- The primary complaint is radial sided wrist pain (base of thumb and dorsolateral aspect of the wrist near the radial styloid process) that radiates up the forearm with grasping or extension of the thumb
- Described as a “constant aching, burning, pulling sensation."
- Aggravated by repetitive lifting, gripping, or twisting motions of the hand (such as opening a jar lid).
- On palpation, some key, significant findings will be tenderness over the base of the thumb and/or first dorsal compartment extensor tendons on the thumb side of the wrist, particularly over the radial styloid process
- Swelling in the anatomical snuffbox
- Decreased carpometacarpal (CMC) abduction range of motion (ROM) of the first digit
- Palpable thickening of the extensor sheaths of the first dorsal compartment and crepitus of the tendons moving from the extensor sheath
- Other possible findings include:
- Weakness and paraesthesia in the hand
- A provocative Finkelstein test
- During this test, the thumb is flexed and held inside a fist. The patient actively deviates the wrist towards the ulnar side. This causes sharp pain along the radial wrist at the first dorsal compartment.
- Osteoarthritis of the first carpometacarpal joint(main differential diagnosis for De Quervain's Tenosynovitis)
- Trigger thumb
- Wartenberg's syndrome (superficial radial nerve neuritis)
- Scaphoid or radial styloid fractures
- Intersection syndrome
Generally, there are three tiers of treatment for De Quervain's:
- Conservative management
- splinting
- ultrasound
- multimodal hand therapy
- activity modification
- Corticosteroid injection
- Surgery
1 and 2 can be combined dependent on patient presentation and willingness to get a corticosteroid injection.
NON-SURGICAL MANAGEMENT:
The aim of non-surgical management is to reduce pain and swelling. Interventions can include:
- Patient education regarding avoiding repetitive or aggravating movements
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Ice/heat packs
- Physical therapy
- Thumb splinting
- Literature supports the use of a forearm brace including the thumb to reduce ulnar deviation and thumb movement.
- Clinicians do not agree on the frequency and duration of splint use; some think it should be worn continually for four to six weeks; others recommend wearing it only as needed for pain.
- Weiss and colleagues found that a 19% improvement was observed when splints were used, but when splint use was combined with NSAIDs, the improvement was 57%. Cavaleri et al. reported that combined orthosis/corticosteroid injection approaches are more effective than either intervention alone in the treatment of de Quervain's disease.
- Ultrasound is thought to improve treatment outcomes and can be used as a diagnostic tool in the management of De Quervain’s disease.
- McDermott et al. found that ultrasound-guided injections were beneficial for De Quervain's tenosynovitis. There results were slightly better than was previously reported in the literature and they reported no adverse reactions.
- Kume et al. found that ultrasound-guided injections which target the Extensor Pollicis Brevis with septation was more effective than manual injection.
- Corticosteroid injection has been reported to be be effective. One or two injections are usually sufficient for pain-relief.
- If there is no significant improvement in symptoms following two corticosteroid injections, surgical management may be considered. Surgery is usually done in an outpatient setting and the anaesthetic may be local, regional or general.
- Patients with moderate to severe symptoms usually require cortisone injections in combination with splinting.
In individuals with persistent symptoms the most commonly non-surgical management includes: splinting, systemic anti-inflammatories, and corticosteroid injection.
SURGICAL MANAGEMENT:
- Surgery is rare and is usually selected in cases where non-surgical treatment has failed and the patient experiences persistent inflammation affecting his or her function. The goal of surgery is to open the dorsal compartment covering to make more room for the irritated tendons. The opening allows pressure relief of the tendons, to ultimately restore free tendon gliding.
- Post-operative care is usually straight forward with a simple dressing and no complicated wound care necessary. Individuals are encouraged to start with early use of the hand for light activities of daily living. Sutures are removed after 14 days and individuals are allowed to continue with normal activities. Mild swelling and tenderness around the surgical site may be present for a few months.
- Ice/Heat Packs
- Heat can help relax and loosen tight musculature, and ice can be used to help relieve inflammation of the extensor sheath.
- Massage
- Deep tissue massage at the thenar eminence can help relax tight musculature that causes pain. The Graston Technique of manual soft tissue mobilisation along with eccentric exercise is also helpful. This technique includes breaking down fascia restriction, stretching connective tissue, and promoting a better healing environment.
- Strengthening
- The progression of exercise therapy is as follows:
- Isometric
- Eccentric
- Concentric inner range
- Radial nerve glides
- Mobilisation
- Mobilisation with movement has shown effectiveness in decreasing the pain, improving range of motion, and improving the function of a patient with De-Quervain's tenosynovitis. The therapist provided a manual radial glide of the proximal row of carpals, then asked the patient to move her thumb into radial abduction-adduction. Mobilisation with movement performed for 3 sets of 10 repetitions and followed by eccentric hammer curl exercise with theraband and high voltage electrical stimulation was shown to be effective at 6 months follow-up. Savva et al. investigated the analgesic effect of joint mobilisation in tendinopathy and concluded that the literature on joint mobilisations in tendinopathies such as De Quervain's remains limited since the effect of these techniques have been sparsely reported in a few retrospective case-series and case studies.
- Taping
- Taping can also be used to decrease pain and improve function.
- Ultrasound
- Therapeutic ultrasound has also better outcomes in pain reduction and healing.
Patients can start with strengthening exercises once their pain has settled to a manageable level. The strengthening programme should be graded and very gradual. Only progress patients through the strengthening programme if they are able to tolerate their current strength programme for at least 1 week. It is important to progress slowly and that patients strengthen in a pain-free range of motion, to avoid aggravation of symptoms. Below are some examples of strengthening exercises.

Comments